Friday, November 22, 2013
Wednesday, October 9, 2013
pain management should be continuous from or to post-anesthetic unit to hospital ward and home
pain service may assist with management of post operative inpatients.
Post-Operative nausea and Vomiting
Some anesthetic agents tend to cause more nausea post-operatively than other (e.g) opioids, nitrous oxide.
Hypertension and bradycardia must be ruled out.
Pain/surgical manipulation also cause nausea.
Often treated with dimenhydrinare (gravol.tm ) metoclopramide (maxeran. tm) (not with bowel obstruction) prochlorperazine ( stematil ,tm) ondansetron (zofran.tm) granisetron.
post operative confusion and agitation .
ABCs first-confusion or agitation can be caused by airway obstruction, hypercapnea, hypoxemia.
Neurologic status (glassgow coma scale.pupils) residual paralysis from anesthetic.
Pain distended bowel /bladder.
Fear anxiety/separation from caregives/language barriers.
Metabolic disturbance (hypoglycemia, hypercalcemia, hyponatremia-especially post TURP).
Sunday, October 6, 2013
Etiology
epidemiology
Wednesday, September 9, 2009
Pleural Effusion
Pleural Effusion
Pleural effusion is an abnormal accumulation of fluid in the pleural space. The 5 major types of pleural effusion are transudates, exudates, empyema, hemorrhagic pleural effusion or hemothorax and chylous or chyliform effusion.
Up to 25 ml of pleural fluid is normally present in the pleural space, an amount not detectable on conventional chest radiographs.
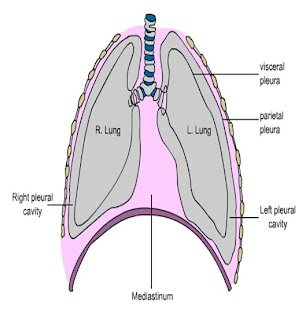
• The pleural cavity contains a small volume of lubricating serious fluid, formed primly by transudation from the pariental pleura and absorbed primarily by the capillaries and lymphatics .
pleural effusion develops when balance between formation and removal of fluid may be compromised by any disorder that
increases venous pressure
lowers the plasma oncotic pressure.
increases capillary permeability.
or obstruct the lymphatic circulation .
General Considerations
Pleural effusions are classified as transudates or exudates to help in differential diagnosis.
pleural fluid protein to serum protein ratio> 0.5
pleural fluid LDH to serum LDH ratio > 0.6
pleural fluid LDH greater than two-thirds the upper limit of normal serum LDH.
Transudates have none of these features
TRANSUDATES ARE CAUSED BY
Decrease plasma oncotic pressure
>Nephrotic syndrome
>Cirrhosis
>Hypoalbuminemia
Increased hydrostatic pressure
>CHF
>Superior vena cava obstruction
Exudates are caused by increased permeability of the pleural surface or by obstruction of the lymphatics .
malignancy
bronchogenic carcinoma
lymphoma
metastatic tumor
inflammatory process
infections:-
- pneumonia
- T.B
- pulmonary embolism
- collagen vascular disease (e.g. rheumatoid arthritis)
- Sub diaphragmatic process
- asbestosis
- pancreatitis
- hypothyroidism
TRAUMA
SYMPTOMS &SIGNS
whereas large pleural effusions may cause
Dyspnea Shortness of breath
Fever
Anorexia general malaise
Pleuritic pain
Cough
Haemoptysis
Shortness of breath
Night sweats
Examination
Decreased movement on the affected side
Tracheal deviation, A massive pleural effusion with high intrapleural pressure may cause contra lateral shift of the trachea and bulging of the intercostals spaces
Stony dullness
Decreased breath sound and vocal resonance
Bronchial breathing aegophony
Look for underlying disease, clubbing ,tar, radiation mark L. Nodes, R.A.etc
LAB INVESTIGATIONS
Leukocytosis with bandemia
PMN predominance:-
Pneumonia,PE, pancreatitis, early TB,abdominal abscess
Mononuclear predominance:-
Tumors, TB.
Blood or air in the pleural space, asbestos, drugs, paragonimiasis
Eosinophil predominance reduces likelihood of TB (10x) and malignancy (2x)
ANEMIA
Pleurocrit/hematocrit >0.5 hemothorax
HYPOALBUMINEMIA
ANTI NUCLEAR ANTI BODY TITER
>1:160 OR> SERUM LEVEL:
Suggests SLE effusion:
RHEUMATIDE FACTOR>1:320 OR >SERUM LEVEL: SUGGESTS RHEUMATIOD ARTHRITIS
PANCREATIC ENZMES
CANCER ANTIGENS 125
CANCER ANTIGEN 19-9
CREATININE/ BLOOD UREA NITROGEN
AEROBIC/ANAERBIC BLOOD/ PLEURAL FLUID CULTURES
Imaging
- CXR
- anteroposterior or PA;
- 75 ml to obliterate the posterior costophrenic sulcus
- 175ml to obscure the lateral costophrenic sulcus in erect position
- 500ml will obscure the diaphragmatic contour , if reaches the level of the 4th anterior rib;close to 1000ml are present


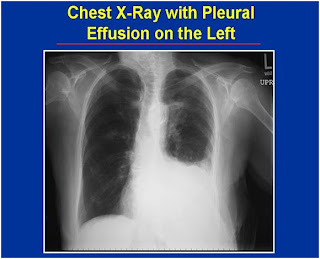
Massive pleural effusion (opacification of an entire hemi thorax) is usually caused by cancer but has been observed in tuberculosis and other diseases.

LATERAL VIEW :-
Small effusion; thinner than 1.5 cm. Moderate ;1.5-4.5 cm thick. Effusion thicker than1cm is usually large enough for sampling by thoracentesis, at least 200ml.

Decubitus view

Pleural fluid may become trapped (“loculated”) by pleural adhesions, forming unusual collections along the chest wall or in the lung fissures

THORACIC ULTRASOUND
Ultrasound is useful to locate loculated or small effusions.


CT SCAN
CT scanning is sensitive in the detection of small amounts of free or loculated pleural fluid.

DIAGNOTIC PROCEDURES/ SURGERY
Diagnostic thoracentesis is not required in small pleural effusion with secure clinical diagnosis or in patients with obvious CHF ,but consider in suspected CHF in following situations;
-Unilateral effusion present ,particularly if it is left sided
-bilateral effusion of disparate sizes
-cardiac silhouette appears normal.
Evidence of pleurisy
Febrile patient
-Alveolar –arterial oxygen gradient is widened out of proportion of the clinical setting


Contraindication for THORACENTESIS
ANTICOAGULATION,BLEEDING DIATHESIS, PT PTT >x2normal ‘,Platelets <25000/mm3>6mg/dl,small pleural effusion,-mechanical ventilation, risk of persistent air leak –brocnchopleural fistula or pneumothoarax.
Initial laboratory tests for an undiagnosed pleural effusion
Protein and LDH in pleural fluid and serum for separation of transudates and exudates
Pleural fluid smears and culture
Cell count and differential
Pleural fluid glucose, amylase, pH
Pleural fluid cytology
Markers for TB pleuritis
ADA, gamma interferon or PCR
EVALUATION OF PLEURAL FLUID WITH DRAWN BY THORACENTISIS
TRANSUDATE has the protein content <30g/l>
An exudate must meet also one the following criteria
>pleural fluid protein/serum protein >0.5
>serum albumin-pleural albumin <1.2g/dl>
>pleural fluid lactate dehydrogenase /serum lactate >0.6
Differential cell count
Absolute cell count not very useful many diseases have WBC above 10,000
Most transudates have WBC <1000>
Differential -polys, small lymphocytes, other mononuclear cells and eosinophils
polys - acute process
mononuclear cells - chronic process
small lymphocytes - malignant, tuberculosis or post CABG pleural effusion
eosinophils
Differential diagnosis of PMN predominant PE with acute infiltrate
Tuberculous pleuritis
Pancreatic disease
Postpericardiectomy syndrome
Intra-abdominal abscess
Viral pneumonia
Lung cancer with pleural effusion
Pulmonary embolism
Lupus pleuritis
Rheumatoid pleural effusion
Drug reaction
Pleural fluid eosinophilia (>10%)
Usually due to air or blood in the pleural space Consider drug reactions
Dantrolene, bromocriptine, nitrofurantoin
Frequent with asbestos pleural effusion
Rarely paragonimiasis or Churg-Strauss syndrome
also low glucose and pH
Frequently no diagnosis obtained
COMPREHENSIVE MICROBIOLOGICAL CULTURING AND GRAMSTAINING /FOR AFB CULTURE AND STAINING.
The Pleural fluid should be evaluated for aerobic and anaerobic bacteria ,mycobacteria ,protoza ,fungi and parasites
Pleural fluid LDH
Not useful in the differentiation of exudates because all exudates tend to have elevated LDH
Very useful when following a patient with a pleural effusion because the level of pleural fluid LDH reflects degree of pleural inflammation
If LDH worsens with serial thoracentesis, process is worsening and one should be more aggressive
If LDH decreases with serial thoracenteses, process is improving
Differential diagnosis -low glucose (<40mg/dl)
Complicated Para pneumonic effusion
Malignant pleural effusion
Tuberculous pleural effusion
Rheumatoid pleural effusion
Paragonimias
Hemothorax
Churg-Strauss syndrome
<30mg/dl>
<60mg/dl>
Differential diagnosis of high amylase pleural effusion; increased
Acute pancreatic disease
Chronic pancreatic disease
Pancreatic pseudo-cyst
Esophageal rupture
Malignant pleural effusion
Pleural fluid pH
Particularly useful in patients with suspected parapneumonic effusion
pH <>
Low pH (<7.2)>
Must be measured with blood gas machine
Pleural fluid markers for tuberculosis
Adenosine deaminase (ADA) >T-lymphocyte enzyme
>High levels also seen with empyema and rheumatoid pleuritis
>Specificity increased if combined with PF lymph/poly ratio greater than 3
Gamma interferon
>Produced by lymphocytes
>Lymphocytes specifically sensitized to PPD produce gamma interferon when incubated with PPD
.PF levels above 140pg/ml are very suggestive of TB
>Elevated whether or not the patient is immunosuppressed
>Is more expensive than ADA
PCR for DNA of M. tuberculosis
If pleural fluid ADA >70 units - diagnostic
If pleural fluid gamma interferon is high - diagnostic
Granulomas on pleural biopsy - diagnostic
If lymphocytic effusion and positive PPD, treat for TB pleuritis if pleural fluid ADA is above 40
If lymphocytic effusion and negative PPD, retest the PPD in 5 weeks - treat if positive
Pleural fluid cytology
Very useful test
1st specimen positive in 60% and if three specimens submitted, may be positive in >80%
Very effective with adenocarcinoma
Less effective with lymphoma, squamous cell carcinoma, mesothelioma or Hodgkin’s disease
Flow cytometry Very useful for demonstrating homogeneity of cells with lymphoma
Immunohistochemical studies ;Monoclonal antibodies are made against various antigens that are thought to be specific for adenocarcinoma, benign mesothelial and malignant mesothelial cells
Diagnostic techniques for tumor markers; There have been many studies evaluating the utility of tumor markers such as CEA, CA 15-3, CA 19-9, and enolase
Collagen vascular disease;
> Rheumatoid pleuritis - useful easy to diagnose
-patient elderly man with rheumatoid nodules
-pleural fluid - low glucose, high LDH, low pH
-must differentiate from complicated parapneumonic
Lupus erythematosus -more difficult
-pleural fluid ANA -probably add little to serum ANA
Chylothorax and pseudochylothorax
with pseudochylotorax, effusion has been present for years and pleura is markedly thicked
If doubt, measure triglycerides and cholesterol in serum and pleural fluid. Chylothorax exists if:
Triglycerides >110 mg/dl and
Pleural fluid/serum triglyceride >1.0Pleural fluid/serum cholesterol <1.0>
PLEURAL BIOPSY if suspicion of TB or NEOPLASM
Closed pleural biopsy should be considered in the differential diagnosis of a pleural effusion that is unexplained after routine studies and thoracentesis. Contraindications include bleeding diathesis, poor respiratory reserve, empyema and absence of pleural fluid.
Open pleural biopsy is sometimes required to establish the diagnosis of pleural malignancy and is especially indicated for the diagnosis of malignant pleural mesothelioma.
Thoracoscopy with a flexible instrument is an alternative procedure with excellent diagnostic accuracy
Treatment
INITIAL STABILIZATION;
Inpatient care is required with this condition.
GENERAL MEASURES
SUPPLEMENTAL OXYEGEN to keep saturation in normal range.
IV Fluid for hydration. Chest physiotherapy.
THERAPEUTIC /DIAGNOSTIC THORACENTESIS.
Treatment should address both the disease causing the pleural effusion and the effusion itself. Transudative Pleural Effusion.
Transudative pleural effusions generally respond to treatment of the underlying condition; therapeutic thoracocentesis is indicated only if massive effusion causes dyspnea.
When bilateral pleural effusions are detected with congestive heart failure, neither diagnostic nor therapeutic thoracentesis is routinely indicated. Such effusions are transudates and will resolve with treatment of the underlying cardiac disease.
ANTIBIOTICS
Empirically by age/social circumstances and modified by blood and pleural fluid culture results.
Empyema ; Antibiotics alone with close monitoring in children. Antbiotics with chest tube drainage in adults.PLEURECTOMY;in cases of trpped lung
Pleural fluid loculation > May inject 250,000 units of streptokinase or hundred thousand units of urokinase intrapleurally to dissolve fibrin meshes creating loculation. If unsuccessful, then either thoracoscopic adhesiolysis or decortication via thoracotomy is indicated.
If effusion is causing dyspnea perform therapeutic thoracentesis, if fluid reaccumulates rapidly place chest tube for continious drainage or chemical pleurodesis with doxy cycline 500 mg, bleomycine 60 units are talc. If pleurodesis fails pleural aberation can be done or pleuroperitoneal shunt and chemical pleurodysis
Chylothorax
>radiation therapy if from malignant cause or surgical repair of thoracic duct trauma.
Hemothorax
> usually caused by trauma or rupture of a tumor drainage through tube thoracostomy.
Steroids and NSAIDs for rheumatological and inflammatory causes
Diuresis for CHF and ascites
Complications
Chronic empyema
Drainage through chest wall: Peurocutaneous fistula
Broncho pleural fistula
Toxic shock syndrome
This article is prepared by Dr Muhammed Naeem Awan

